Case Study: Shockwave Therapy for Plantar Fasciitis in 47 Year-Old Male Runner
Presentation: plantar fasciitis
A 47 year old male presented to the Sydney Heel Pain Clinic requesting plantar fasciitis treatment. He reported heel pain in both feet for at least 7 or 8 months. He was otherwise fit and healthy. The patient told the sports podiatrist that he had increased his running distance lately and he had added 2 extra training days in preparation for his workplace charity fun run. He was running 6km five days per week when the plantar fasciitis kicked in.
Pain symptoms were consistent with plantar fasciitis
When asked to describe his pain from the plantar fasciitis, the patient said it was very sharp and deep in the centre of the base of his heel. He said that his heel pain was always very bad first thing in the morning when he got out of bed but usually subsided after a few minutes of walking- a classic sign of of plantar fasciitis. The patient told the sports podiatrist that he was able to run with bearable pain after around 5-10 minutes of starting. The patient was particularly concerned that once he had finished running, his heel pain would become severe.
The patient had tried some home remedies for plantar fasciitis
The patient informed the sports podiatrist that one of his colleagues had mentioned he may have plantar fasciitis, and based on that, he had done some reading on the internet which led him to try some home remedies to relieve his heel pain. He had been using ice packs to ice his feet following his training. He had also purchased some over-the-counter orthotic inserts that the pharmacy assistant had suggested may be helpful for plantar fasciitis. He confessed to the sports podiatrist that these orthotics were actually quite uncomfortable and he did not wear them consistently.

Evaluation of plantar fasciitis in the patient
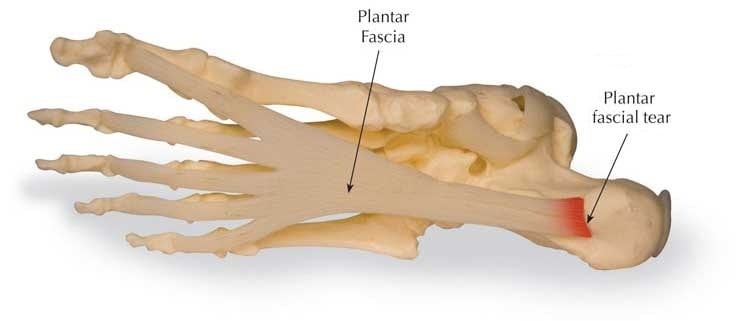
A thorough physical examination was carried out by the sports podiatrist in order to evaluate the severity of the plantar fasciitis. The patient reported a lot of pain around the plantar aspect of the heel as the sports podiatrist palpated his foot. This is the area where the plantar fascia ligament attaches to the heel bone. The sports podiatrist discovered that the patient also had tight calf muscles in both legs, which was limiting the range of motion in the patient’s ankles, hence putting pressure on the plantar fascia. The sports podiatrist informed the patient that his signs and symptoms were consistent with a diagnosis of plantar fasciitis.
Biomechanical assessment for plantar fasciitis
A biomechanical assessment and gait analysis was carried out during the initial consultation as part of the examination for plantar fasciitis. The biomechanical assessment is a useful tool in assisting the sports podiatrist to identify malalignments, imbalances and abnormalities in the patient’s legs and feet as they walk. This information is often used to form the basis of the treatment plan, since plantar fasciitis is often caused by chronic overuse of the plantar fascia ligament due to suboptimal gait. The patient’s arch height and heel position were also measured.
Plantar fasciitis treatment for the patient
A treatment plan was devised for the patient’s plantar fasciitis, with the aim being to reduce inflammation and relieve heel pain, whilst allowing the plantar fascia ligament to heal. The sports podiatrist devised a treatment plan comprised of three main components:
- Stretches for the tight calf muscles
- Custom-made orthotic inserts
- Shockwave therapy.
The patient was prescribed a series of particular stretching exercises by his sports podiatrist. The exercises were particularly selected to assist with increasing flexibility in the calf muscles, which would reduce the strain on the plantar fascia and therefore allow the ligament to heal.
Custom-made orthotics were ordered for the patient. These would assist in the healing of his plantar fasciitis by controlling and supporting the arch of the foot, without putting too much pressure on it. The patient was advised that he would need to wear the orthotics every day for 6-8 weeks. In this time frame, it was expected that his heel pain would resolve and the plantar fascia ligament would begin to heal.
Shockwave therapy treatment was scheduled for this patient once a week for four sessions. Shockwave therapy is a scientifically proven treatment for plantar fasciitis. It works by directing high frequency sound waves into the area, which stimulates blood flow, tissue regeneration and breakdown of scar tissue, whilst also providing almost instantaneous pain relief.
The patient was advised by his sports podiatrist that he would need to refrain from running for the next 3 to 4 weeks whilst he underwent his treatment for plantar fasciitis. The sports podiatrist suggested that in the meantime, he could walk or lightly jog for short intervals only, provided that he followed his prescribed stretching regime closely.
Shockwave therapy for plantar fasciitis treatment: the outcome
The patient returned to the clinic one week after his initial consultation, to have his custom orthotics fitted and to receive his first shockwave therapy treatment. The patient reported immediate pain relief at the cessation of the first shockwave therapy treatment.
The patient’s following shockwave therapy treatment for plantar fasciitis was scheduled for one week later. He informed the sports podiatrist that whilst he’d experienced immediate pain relief following his last treatment, the following morning he had the same severe heel pain. The sports podiatrist reassured him that this was normal and that the therapy can take a number of sessions to take effect. His second shockwave therapy treatment also provided him instantaneous pain relief. At this second therapy session, the patient also reported that he was becoming accustomed to wearing his orthotics. He had been compliant with the stretching regime that the sports podiatrist had prescribed for him.
The patient received two more shockwave therapy treatments for his plantar fasciitis in the following two weeks.
The patient returned to the clinic for a follow-up consultation with the sports podiatrist eight weeks from the initial consultation. The patient reported that his pain from plantar fasciitis had almost completely resolved. The sports podiatrist advised him that he could begin to run again, only over short distance intervals to begin with. He was told to slowly increase his running distance (by no more than around 10% per week).
Please bear in mind that this case study is unique to the individual patient as described. Treatment details should not be taken as general medical advice. If you are suffering with plantar fasciitis or any type of heel pain, you should consult with a qualified sports podiatrist for an accurate diagnosis and individualized treatment plan.
Podiatrist Karl Lockett
Sydney Heel Pain Clinic
93883322
help@sydneyheelpain.com.au
Written by Karl Lockett


 Plantar Fasciitis Home Remedies Tried by the Patient
Plantar Fasciitis Home Remedies Tried by the Patient